Temperature charting can be a powerful addition when charting your menstrual cycles, however it is not always an infallible biomarker.
There are two main reasons why temperature can lead to a false “ovulation” confirmation – both of which we’ll cover in detail.
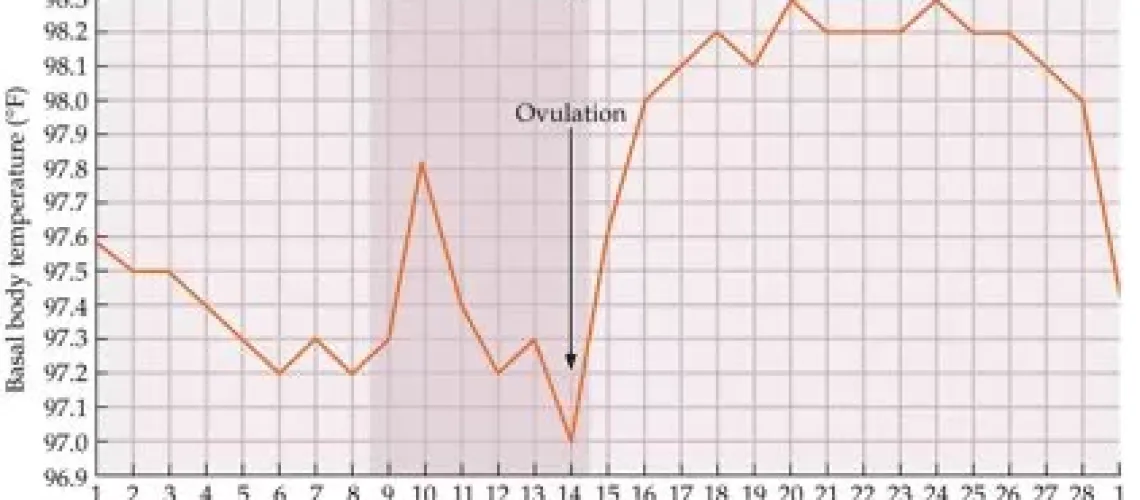
For some background, there needs to be an understanding on why we use basal body temperature (BBT) charting as part of fertility awareness or natural family planning. It is commonly understood that the reason charting your BBT can help you detect ovulation is because once ovulation has occurred and the follicle restructures itself into the corpus luteum, progesterone production begins.
Progesterone has a thermogenic effect on the body and it is believed that we see an increase in BBT after ovulation has occurred.
However, that is not strictly true. The reality is progesterone production can begin before ovulation occurs. This is because initial progesterone production is triggered by high levels of luteinising hormone (LH). Then, once ovulation has occurred the corpus luteum produces additional progesterone. This is why methods that utilise BBT have strict rules that need to be met in order to confirm that ovulation has occurred.
Now that you understand the basics, let us talk about false temperature spikes. Basal body thermometers measure to such a precise number (two decimal places) that external factors can impact our temperature and in turn, our charts. The list of things that can impact your BBT readings is extensive and as a rule if it is outside your ‘normal’ (for example alcohol or drug consumption), an inflammatory response (for example hay fever) or an immune response (for example having the flu) you can expect that it may impact your BBT.
The following is by no means an exhaustive list, but a few things that can cause disruption in your BBT charts:
- Alcohol or drug (medicinal or otherwise) consumption
- Travel
- Stress
- Illness or injury
- Flu/common cold
- Sporting injury
- Allergies/hay fever
- Sunburn
- Recovering from an operation
- Hot/cold bedroom or sleeping area – our bodies are typically pretty good at regulating
throughout the seasons, so you may see no real difference between your temperatures from
summer to winter, however if you have one night that is extreme you may notice it reflected
in your charts. This is often due to restless sleep, rather than the outside temperatures. If you do notice a temperature spike, but have no other signs of ovulation (cervical mucus changes, positive luteinising hormone tests) and you have experienced a departure from your normal, it would be wise to mark the disturbance on your chart and proceed with caution.
Now let’s talk about those instances when temperatures may not behave. It is a very commonly held belief that the luteal phase of your cycle (from ovulation to menstruation) is fairly stable, and that 16+ days of high temperatures are often a fairly reliable sign of early pregnancy. However, there are times when this is incorrect.
Luteinised Unruptured Follicle
A luteinised unruptured follicle can occur when LH levels are high enough that progesterone production begins, however ovulation is unsuccessful. From a charting point of view, it can look like ovulation has occurred but no egg has been released. This can occasionally be detected by lower-than-normal temperature shifts, however sometimes BBT readings can appear as normal.
Corpus Luteum Cyst
Corpus Luteum Cysts develop on the corpus luteum and prevent it from breaking down, so while ovulation has successfully occurred progesterone production continues beyond what might be normal for the individual.
In both of these hormonal events temperatures can stay high beyond 16 days. If intercourse has occurred at any point in the cycle and pregnancy tests are negative it is an indication that the individual may be experiencing a luteinised unruptured follicle or a corpus luteum cyst. These can resolve on their own, however they may also require medical attention. Throughout your reproductive life you may experience one, or both, of these and while they can be annoying (and sometimes painful), it’s not really cause for concern. If it is a recurring event then further investigation may be required.
The best part is that if you’re charting your cycles you can very quickly detect if something is amiss, you can make a fully informed decision about your care and you can arm yourself with all the information needed to seek out help!